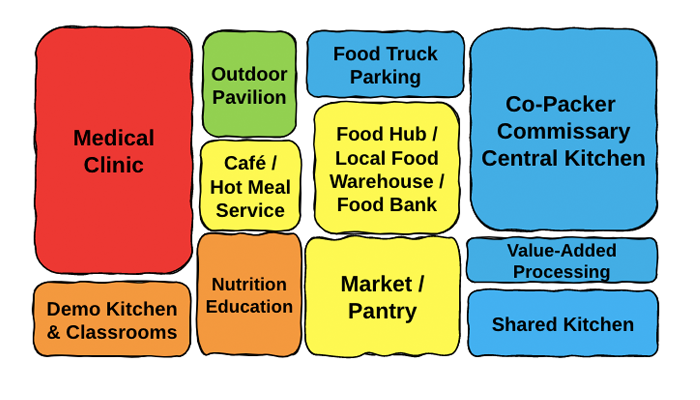
Community Food Centers (CFC) are an exciting development in food system infrastructure and make up an increasing share of our work at New Venture Advisors. Typically this facility or group of facilities is composed of multiple types of food enterprises, each with a distinct, dedicated space. Together, there are naturally-occurring synergies that benefit each enterprise and the communities around them.
We are excited about a trend influenced by the “Food as Medicine” movement. CFC operators are partnering with medical providers to co-locate health and wellness services with other types of food enterprises in one or an adjoining facility. This seemingly simple addition turns a CFC into a CFHC, Community Food and Health Center, and elevates the benefit of both sides, especially in under-resourced areas.
Balancing Missional and Financial Goals
CFCs often have a strong social mission guiding strategic, tactical, and operational decision-making. For some, this mission involves supporting small and midsize food producers; others focus on providing consumers with affordable access to healthy food. Unfortunately, reconciling socially-motivated and financial objectives can be difficult.
While food centers play a pivotal role in strengthening regional food systems, often they are not profitable because they lack scale as they work with small businesses and producers. Ultimately a CFHC promotes a comprehensive response to local food access, small farmer market access, and nutrition-based health issues that mutually benefit agricultural producers and consumers.
Medical groups are valuable anchor tenants as they can attract additional financial resources and consumers. For example, medical groups are often attached to hospital systems with funds set aside for community investment projects. In addition, more grantmakers are interested in collaborations that promote medical care access. Note: It is important to involve healthcare providers at the beginning of the project, as many have specific space requirements to meet HIPAA compliance standards.
Addressing Social Determinants of Health
Given what we know about the impact of food insecurity on individual health and the healthcare system, a CFHC can make a huge stride in improving equal access to healthy foods for communities that face many social determinants of health, a set of conditions in which people are born, grow, live, work, and age that shape their health.
Even the USDA acknowledges the benefit of food as medicine and added $40 million to the GusNIP Produce Prescriptions Program. GusNIP is based on the reality that many prevalent health conditions stem from nutrient-deficient diets. This program funds projects demonstrating the impacts of fresh produce prescriptions to increase fresh fruit and vegetable consumption, improve health, and reduce food insecurity. Since launching this program in 2018, the number of applicants has increased by 30 percent yearly.
If medical practitioners continue to make referrals for fruit & veggie prescriptions and medically tailored meals, it makes sense to create a one-stop shop. Referred patients are often required to complete cooking classes and nutrition education and provide regular health metrics. If these programs, along with flexible food distributions, can occur in the same place where people receive medical care, it could increase participation and decrease access barriers. Also, it could provide the education many clinicians need on the appropriateness and use of these interventions.
While medical clinics may be a prominent partner for a CFHC, there is also a wider interpretation of health our clients embrace. For some, a healthy community means decolonizing their diet, reintroducing cultural crops, and training the next generation on lost traditional food preparation knowledge.
Many of these projects are in the early stages, but we think the concept is valuable and essential. Stay tuned to our case studies as we share out the innovative ways clients are incorporating a food and wellness approach to their projects.